The thing about statistics is, they will not tell you how a specific person, in a specific circumstance, will react under certain conditions. However, statistics and good solid info will help you make a decision relative to the associated risks.
Uterine rupture does happen, and here, we discuss what the REAL risks are so YOU can make the best decisions for your birth.
Up to 80% of women who attempt a VBAC will be successful, and VBAC is generally associated with fewer complications than a repeat Cesarean.
The biggest risk and the most influencing factor for VBAC is uterine rupture. A uterine rupture is defined as a tear through all three layers of the uterine lining.
However, uterine rupture can even occur in women without a prior Cesarean, albeit not as likely (0.07%), or one in 1,146 pregnancies.
Uterine Rupture vs. Uterine Window and Dehiscence
Uterine rupture is rare, although it does happen; uterine dehiscence is often mistaken and classified as a uterine rupture.
Uterine rupture is when the uterine scar completely opens along the scar going through every single layer of the tissue. A dehiscence is when a very small amount of the scar begins to separate but doesn’t quite make it the entire distance.
A uterine window is when the scar is so thin that you can see through it but it does not tear or open.
After a Cesarean, our bodies heal and create scar tissue. That scar tissue is not as stretchy as our original tissue, but it still has the ability to stretch.
Uterine Window
As your baby grows, the uterus stretches and can become thin. A uterine window is a thinning of the uterine wall where it has stretched to accommodate a growing baby, as opposed to uterine dehiscence where the scar begins to separate.
In order to know if you have a uterine window, a Cesarean would need to be performed or an ultrasound may show the thinning. Your provider would be able to tell you during the Cesarean because of how thin it would look.
Evidence has not shown thus far if a uterine window is an indication that a rupture would be more likely or not. A lot of parents will likely go on and VBAC without knowing if their uterine lining ever was thin.
Uterine Dehiscence
There are three layers to the uterus. If the uterine scar opens partially, stretching the scar tissue and opening the bottom layer, this would be classified as a uterine dehiscence.
Uterine dehiscence is often harmless and doesn’t have any harmful effects on the baby or the mother.
A 10-year Canadian study was done on full uterine rupture vs. uterine dehiscence. Over the 10 years, there were 114,933 deliveries with 39 cases of uterine rupture: 18 complete and 21 incomplete, or dehiscence.
Uterine dehiscence did not have any fetal deaths. Uterine rupture is a scary topic for providers. It can often be hard for women to be able to find a supportive provider for VBAC due to this fear.
How to Determine Uterine Dehiscence
As with the uterine window, a repeat Cesarean would need to be performed in order to confirm uterine dehiscence.
Historically, providers would explore the uterus more during a Cesarean to see if there were any other tears, but currently that practice is not likely to happen.
Taking the mother’s pulse rate carefully and consistently during labor may be the only sign that uterine dehiscence is happening or has happened.
When the scar tissue starts to separate, fluid can enter the body cavity and leak into the membrane that separates the organs from the cavity wall. When this happens, the body reacts with shock and the mother’s heart rate may increase dramatically.
In the same 10-year study, in 92% of cases, uterine rupture was associated with previous Cesarean delivery (Kieser & Baskett, 2002). Uterine dehiscence was associated with minimal maternal and perinatal morbidity.
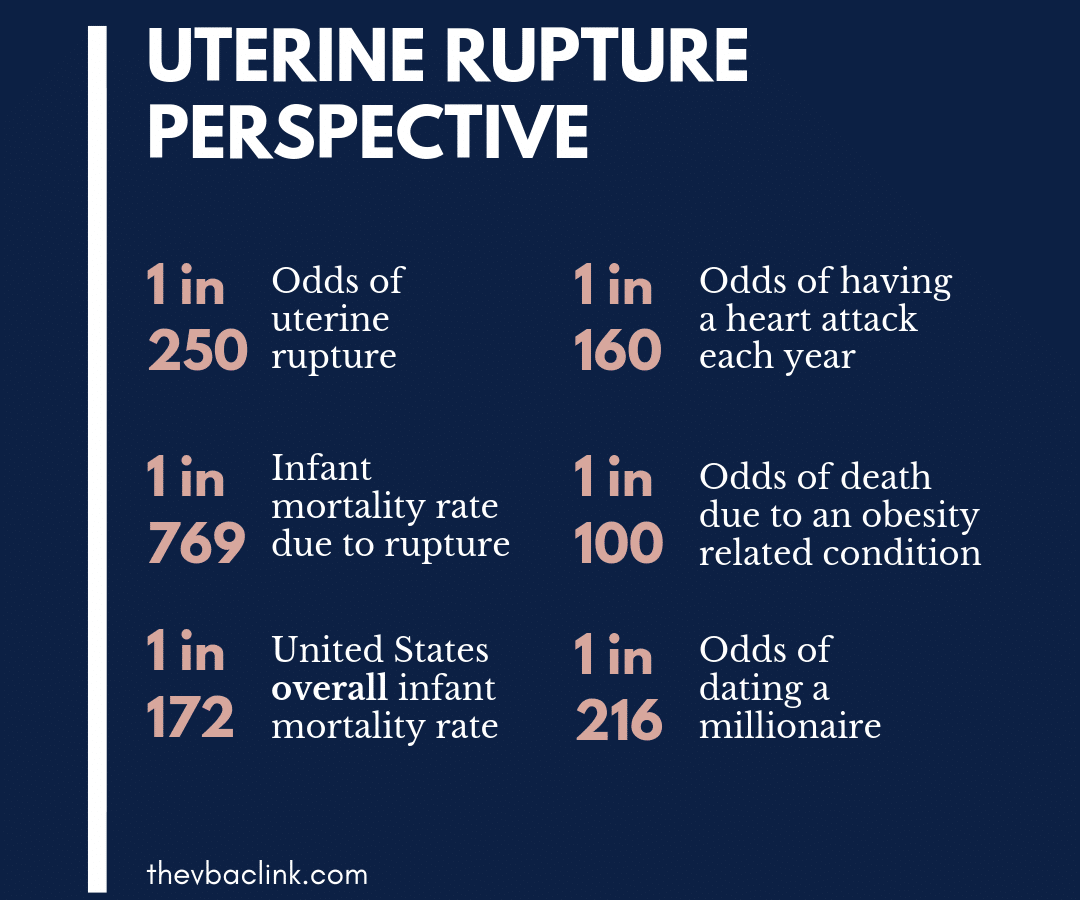
Putting Uterine Rupture into Perspective
Statistically, uterine rupture happens in 0.4% of TOLAC. That equals one in 240.
Now, as will all things, probability should be considered and assessed. When uterine rupture does happen, most of the time it is quickly detected and a provider is able to get the baby out quickly (usually by repeat Cesarean) before any long-term damage happens to the mom and/or baby. In fact, only 6% of uterine ruptures are complete or catastrophic.
“The overall risk of perinatal death due to uterine rupture was 6.2 percent. The two studies of women delivering at term that reported perinatal death rates report that 0-2.8 percent of all uterine ruptures resulted in a perinatal death.” (Guise, et al., 2010)
To put it differently, of the women who had a uterine rupture, one in 16 resulted in infant death.
When looking at the overall chances of infant death when attempting a VBAC, the National Institute of Health (NIH) reports the odds as 0.13%, which ends up being one infant death in every 769 TOLACs.
For comparison, the average neonatal mortality rate for the U.S. in 2014 was 5.8 per 1,000 births. That’s one in approximately 172.
Just for fun, and because I am a statistics geek, let’s take a look at some things more likely and a little bit less likely to happen to you than a uterine rupture:
- 1 in 160 – Chance of having a heart attack each year (CDC, NCHS, 2021).
- 1 in 216 – Chances the person you are dating is a millionaire (Baer, 2003, Life: The Odds).
- 1 in 5 – Chances of your death being due to heart disease (CDC, 2024).
- 1 every 18 years – How frequently you will be in a car accident (Property Casualty Insurers Association of America, 2018).
- 1 in 30 – Odds of conceiving twins (Martin, Hamilton, Osterman, Driscoll, & Drake, 2018).
- 1 in 300 – The risk of cord prolapse (Lore, 2018).
- 1 in 160 – Odds of being audited by the IRS (Heath, 2018).
- 1 in 199 – Odds of falling to your death (McCarthy, 2018).
- 1 in 14 – Odds of having your identity stolen if you are 16 years or older (Datko, 2013).
- 1 in 100 – Odds of dying from an obesity-related conditions (Allison, Fontaine, Manson, & Stevens, 1999).
- 1 in 38 – Chance of developing melanoma (American Cancer Society, 2018).

Reducing the Risk of Uterine Rupture
There are many things you can do to minimize the chances of uterine rupture. It is important to discuss these things with your provider and have a solid plan ready if any interventions are necessary.
- Stay away from induction unless absolutely necessary.
- Avoid augmentation of labor (something to stimulate contractions, usually Pitocin).
- Avoid excessive Pitocin and upping the dose too fast.
- Avoid Cytotec (misoprostol) COMPLETELY.
- Avoid providers who aggressively intervene with and manage labor.
- Stay mobile. Walk, change position and posture when in active labor.
- In early labor and if labor stalls, rest or sleep.
- Do EVERYTHING you can to make sure your baby is in the most optimal position BEFORE labor begins.
- If baby is not in a great position and labor stalls or you have back labor: try spinning babies, MILES circuit, abdominal lifting, side lying, or get on hands and knees to try and help baby settle into a better position.
- Avoid rupturing membranes if baby is not in optimal position.
- Avoid an epidural if possible.
- Have attentive labor support with you ALL THE TIME.
- Be aware of typical labor patterns. Any stalls in labor are usually indicative that something needs to change (emotional processing, baby position, rest/sleep, and even Pitocin in some instances). Figure out what needs to change and fix it if you can. A long stall combined with high doses of Pitocin is a prime scenario for uterine rupture.
- HONOR YOUR INTUITION. If you feel that something is not quite right or if baby’s movement is significantly decreased, insist that your provider or their staff attention to you. In many instances, uterine rupture occurs when a mother knows something is wrong intuitively before providers pay sufficient attention.
Check out special episode 08 of our podcast to listen to Julie and Meagan talk all about uterine rupture and what signs you need to be aware of.
Listen to our friend Heather on episode 56 of the podcast to hear her experience with a uterine rupture.
Interested in becoming a doula and helping women through their birth experiences? Register today for our Advanced VBAC Doula Certification Program, and learn everything you need to know to pursue a new doula career — from the comfort of your living room.
This video-based online course offers the world’s most comprehensive VBAC doula training program, with the knowledge and resources you need to get certified and start practicing.













 Meagan’s VBA2C Birth Stories
Meagan’s VBA2C Birth Stories
Hi. I had a question. I was wondering how likely a successful VBA2C would be? I’ve had a vaginal birth in 2016(no complications baby was 36 weeks), an emergency csection in 2017( placental abruption, prolapsed cord and water broke baby was 28 weeks and had died before reaching the hospital), a vaginal delivery in 2018(baby had passed away at 18 weeks), in 2019 a repeat csection (baby was head down in the birth canal and I was having contractions and had been in labor for 6 hours prior coming to the hospital without knowing I had extra fluid due to developing gestational diabetes so I didn’t recognize the contractions that morning neither one of us were in distress-unneed csection in my opinion) and now I’m due with my final baby in April of 2021. I’m absolutely terrified of csections, the operating room, even just hearing the words csection makes me start shaking. I’ve had two people tell me that a csection is recommended but I feel like I could successfully do a VBA2C with both baby and I safe. Any advice? Tips on trying to make sure it’s successful and maybe convince my provider to let me try without transferring me to someone else who is over an hour away? I’m considered high risk(cerclage and progesterone suppositories-suppositories are weekly when I hit 16 weeks and I’ll be seen every 2 weeks to keep an eye on my cervical cerclage via ultrasound). Thank you in advance 😊
Hello!
I just came across this article and it’s very educational, thank you for it!
I do have a question/advice to ask
Three years ago to the dot, i was having my third birth, my second via c section. Previous to that i had another c section, and before that, a very successful first vaginal birth.
During this second c section (that had no complications whatsoever) the Dr told me while putting me back together, that I had a uterine window and that she will recommend me not having more children.
Today, three years laters, i haven’t been able to made peace with this. I long for a baby so so much.
I know a Doula who is an aunt of of the country and she said that my body should heal if i give it time, she actually said that I could wait until my baby turns three, which is tomorrow (from the day I’m writing this), and that i should be fine. I’ve had an IUD since my daughter was 2 months and I haven’t taken it out. I will not chose to have another pregnancy if i know I could be in danger of leaving my children without a mother or a future baby not making it. But i seriously I’m heart broken about not feeling like we have all of our famio complete, i feel like I’m missing a baby.
A little bit of my history my first pregnancy was very healthy no problems whatsoever vaginal birth and then I had a miscarriage around 7 weeks pregnant and then I got pregnant of twins and they were born at 38 weeks perfectly healthy No complications whatsoever and that was my first C-section and then I got pregnant again and then I had my daughter with another C-section cuz she was breach and it was during that C-section that the doctor said to me about the uterine window.
I don’t have any other problems like high cholesterol or high blood pressure I’ve never had the stational diabetes any problems whatsoever the only thing that is stopping me from getting pregnant again is this information that I have and the fear that I will die on that table leaving my children alone but I’m so desperate and I’ve been looking for some answers and some direction and advice of what I need to do do you have any words for me.
Listen, I’m on my 7th pregnancy (9 if you count my two miscarriages) I’ve had 5 CS’s and 1 successful VBA2C. My 5th was a VBA3C, but unfortunately I had an incomplete uterine rupture during the labor and delivery. In that CS, the dr told me I had a window and I shouldn’t try to VBAC again. I had my 6th child 3 years after that and CS @ 36 weeks to avoid a complete rupture. The operating Dr said that my window was so thin, she could see the baby…”this is your last one”. I’m 38 years old and 25 weeks pregnant. I have been burned by enough drs to know when I’m being bullied. Yes, I have a very thin window, and yes I’m at risk for another rupture. But I wasn’t done having babies. I have taken care of myself, I do not have any health risks & neither does my baby. I’m being closely monitored (actually, I see Maternal Fetal Medicine every 8 weeks and my regular OB every month as normal. They are pushing me to have another 36 week CS because they don’t want me to labor. I’ve pushed back on them to 38 weeks because I’ve NEVER had early labor. I also know that I can run to the hospital if I do go into labor.
My advice to you is find a different Dr. I drove almost 3 hrs to the right dr because he would VBAC. And it was totally worth it to me. You shouldn’t be bullied. Multiple pregnancies are possible with a “window”. My biggest fear is dying and leaving my 6 kids without their mom. But I have done research, I am working closely with my drs, and we have a plan in place. Work with your dr to have a plan. My dr has me going to a hospital (an hour away from where I live) because they have the NICU, blood supply, and around the clock drs. She also said if I wanted to plan to do it closer to my home, THEY will plan to have blood ready at the hospital IN CASE. YOU CAN DO THIS!! YOU CAN HAVE MORE BABIES!! Be strong, be confident, seek a Dr who is willing to try! They are out there!! Good luck and God bless your efforts!! ❤️❤️
I really needed to hear this. thank you so much. I’m going through something similar and I’m trying to not allow the Drs to break me. all I’m hearing is how I’m going to die or how they have to take my uterus out. I Have 5 kids and is on my 6 all CS. and trying to find all my options.
Hey Gretchen… wow, we are so sorry that you’re feeling lonely as you navigate this. We are so glad you’re hear and hope you’ve found our information to be helpful. We have several other good articles that I think you’d appreciate, like this one on vaginal birth after multiple cesareans. You can also find so many inspiring real birth stories on our podcast. AND – be sure to consider taking our How to VBAC: The Ultimate Prep Course for Parents. It’s self-paced, completely online and is packed with a ton of info about the risks, stats, encouragement and so much more to support your VBAC journey. Feel free to email us at info@thevbaclink.com for a discount code. We’re rooting for you!!!
Thanks so much for this article! I just discovered your blog and podcast, and look forward to learning more to prepare myself to attempt a VBAC! I have a question about uterine rupture that I can’t find the answer to anywhere. When it happens during a VBAC, does the tear happen right on the scar, because it’s not strong enough, or right beside, because the scar isn’t pliable enough? I’ve had discomfort asking my scar both before and during this subsequent pregnancy. Before becoming pregnant, I dealt with it by massaging with essential oils to help the skin stretch and become softer, and going to an osteopath and acupuncturist who worked on the scar tissue. Since becoming pregnant, I haven’t done the acupuncture, and my osteopath doesn’t do much with my scar anymore. I’m trying to figure out whether applying oils to encourage stretchiness is a good or bad idea! Any advice?
HI! Thank you so much for your comment and question. It is a really great one!
Unfortunately, when uterine rupture happens it can vary, but usually, it is the scar itself that is separating. It is common to feel pressure in the scar area during pregnancy and even labor but it is really important to look out for the other symptoms. If you had discomfort it may have been scar tissue/adhesions pulling. Sadly what providers don’t talk about often is even years and years down the road CS scars should be massages and worked with. Lynn Shulte who we have had on our podcast actually talked about this in an episode. I will drop the link below.
https://www.youtube.com/watch?v=p-VfUJ6JcWo
Check out episode 123 on Spotify or Apple.